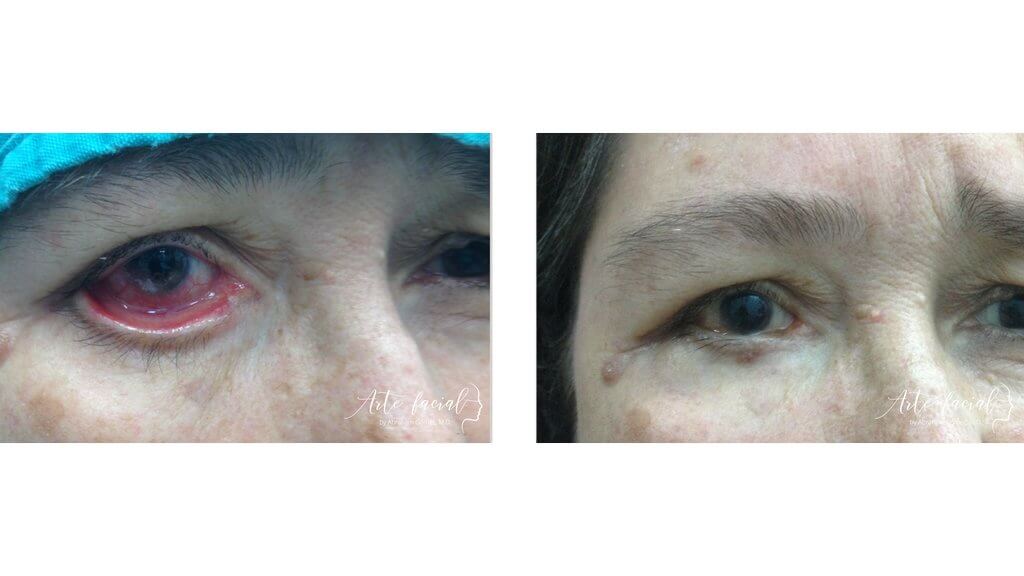
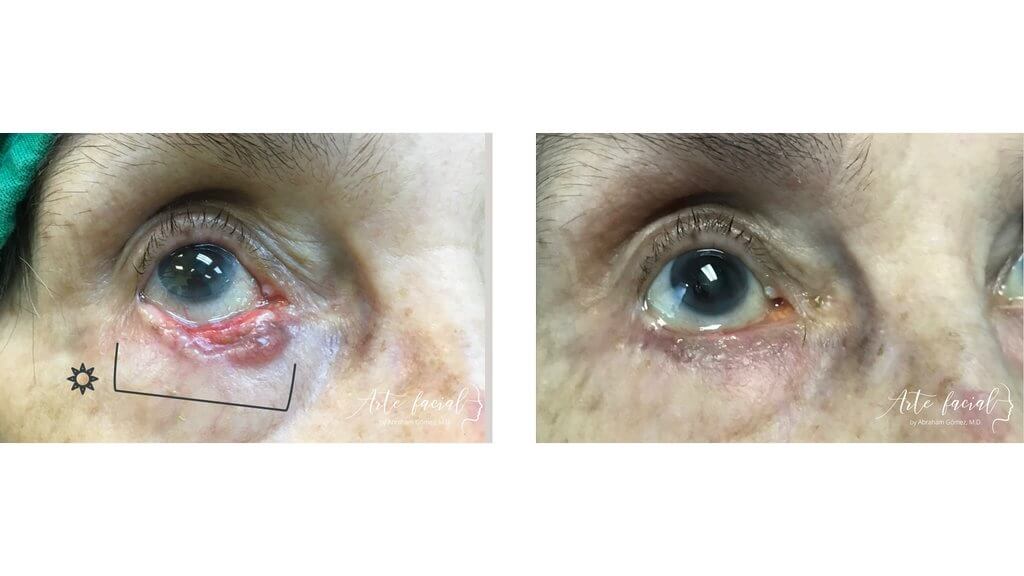
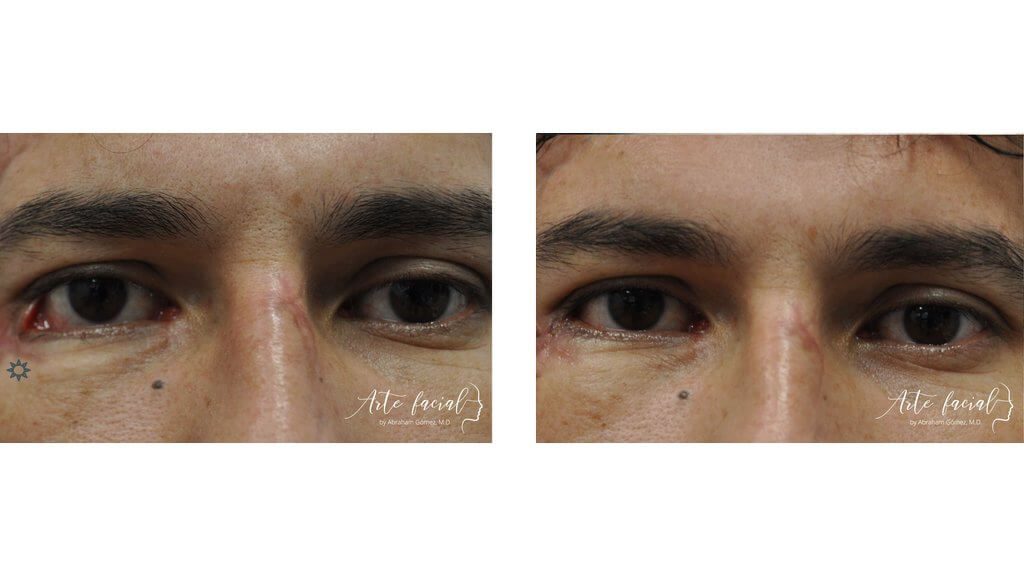
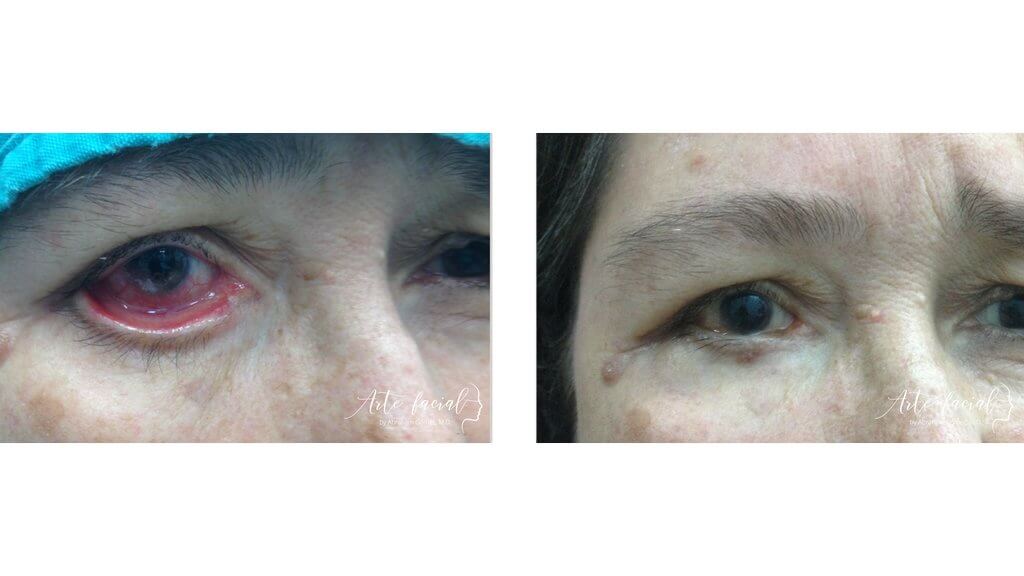
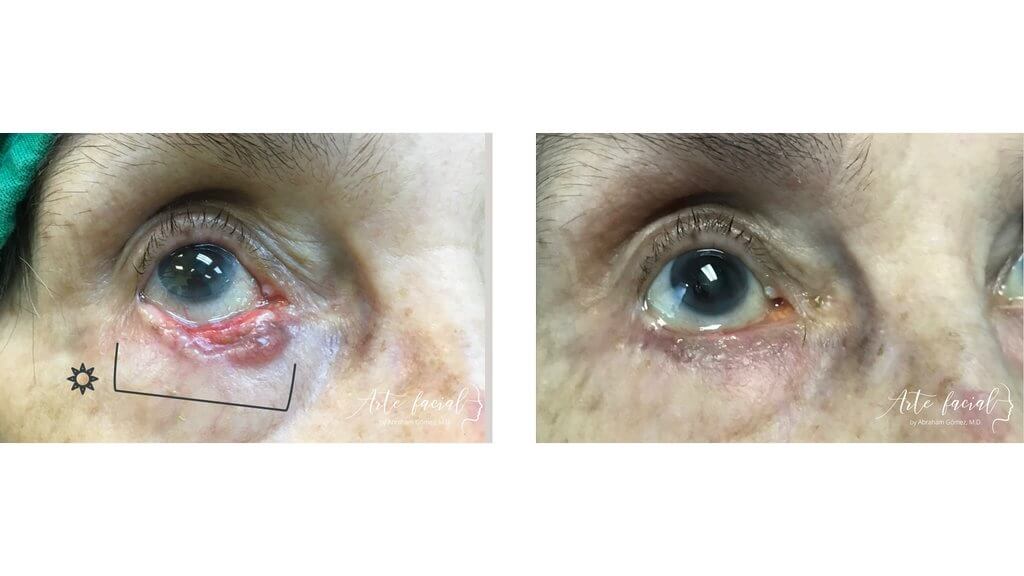
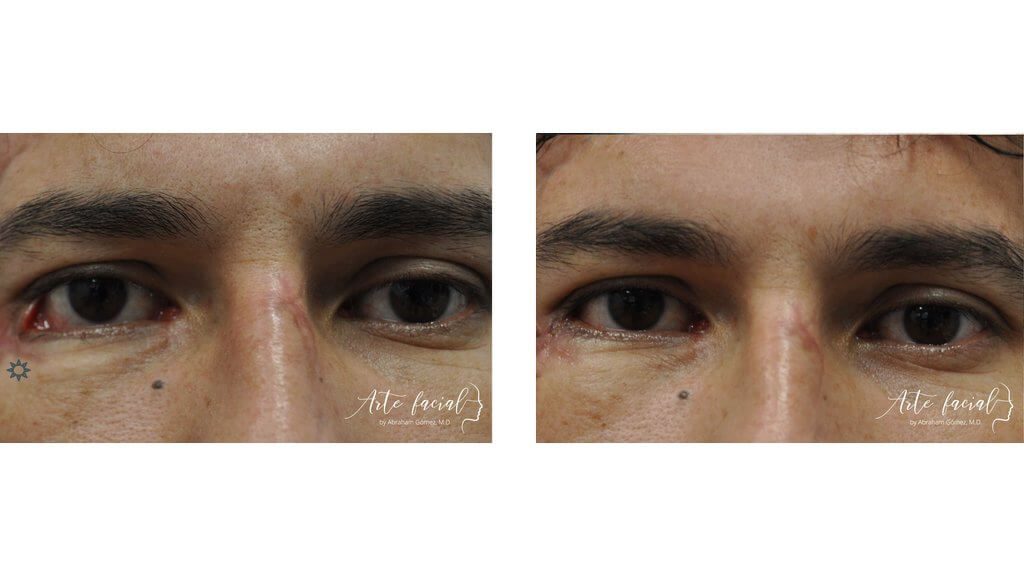
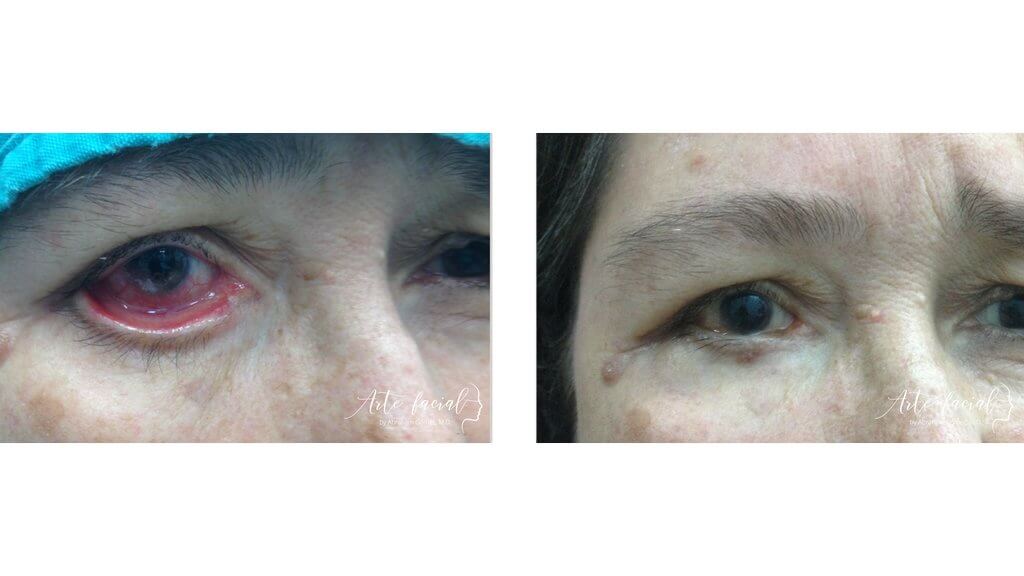
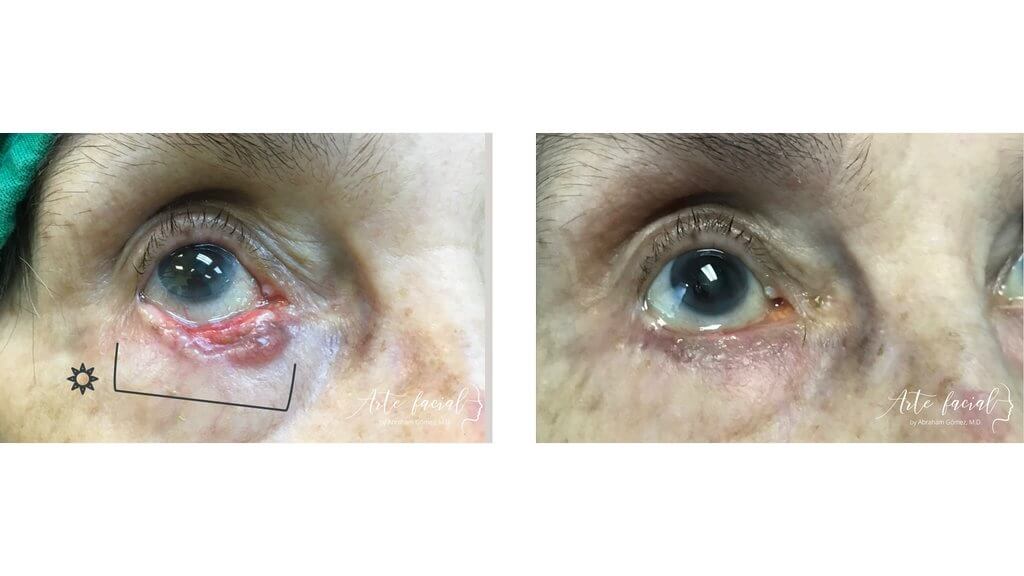
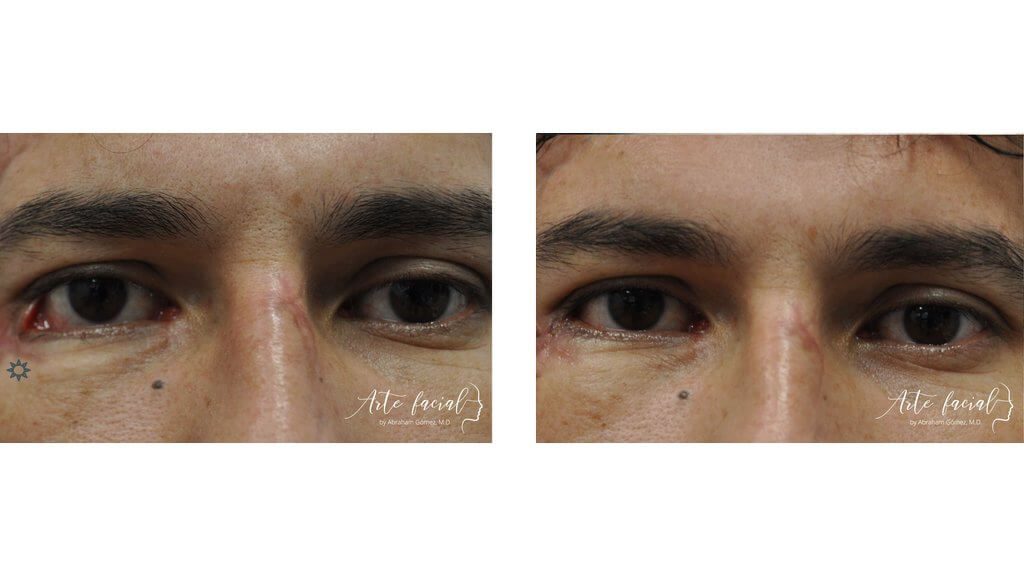
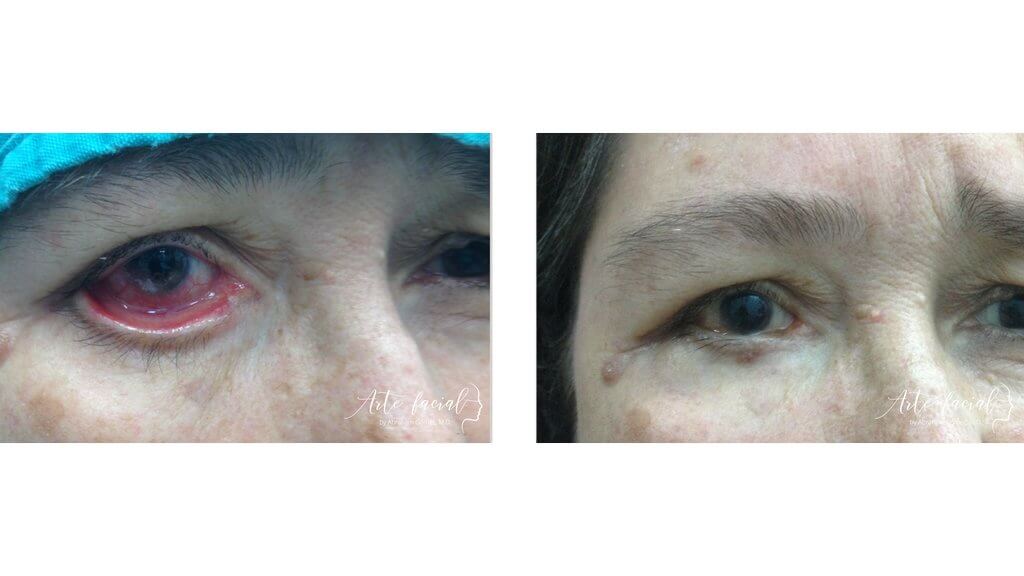
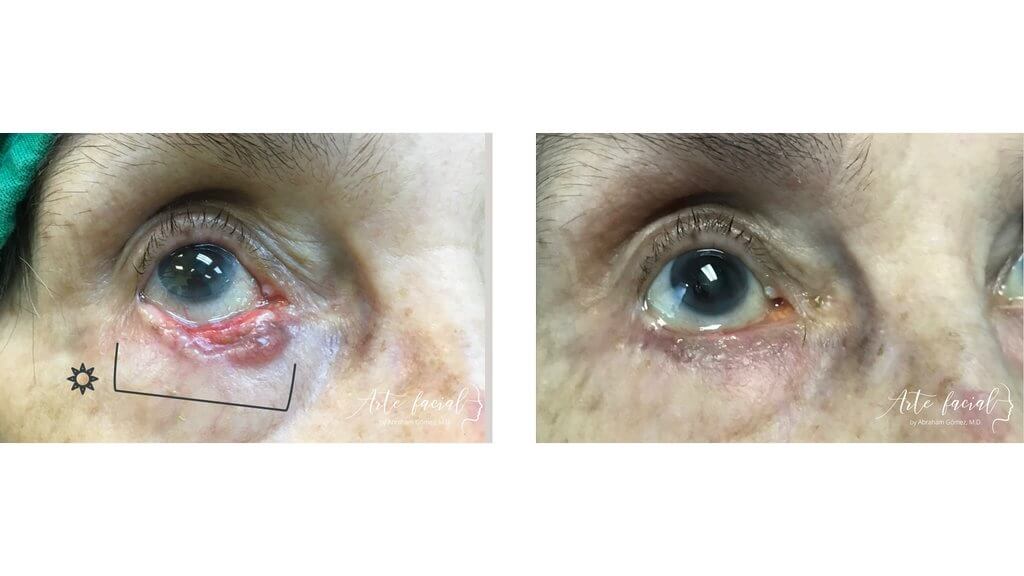
Before
After

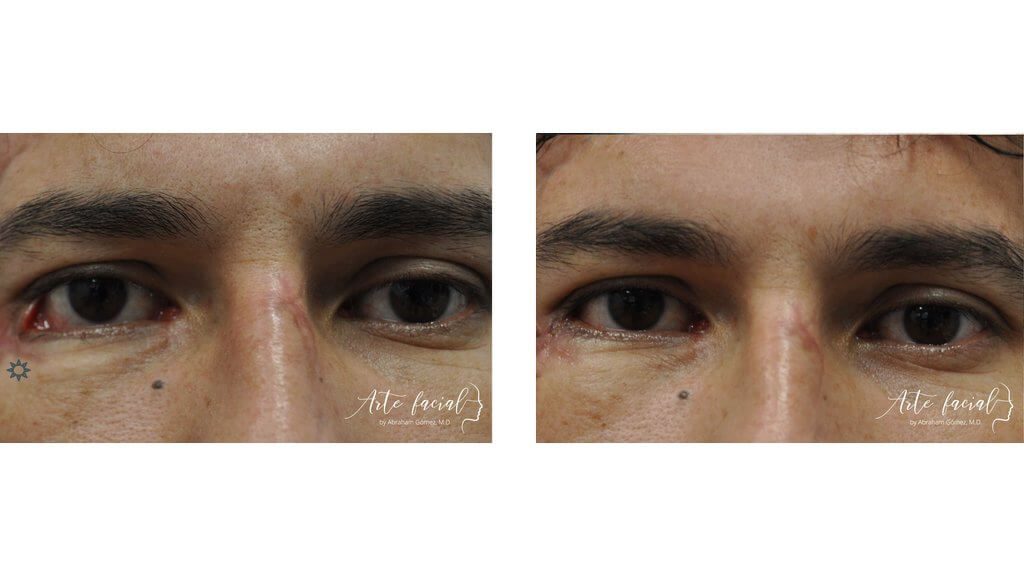
Functional & reconstructive (3)
Functional & reconstructive (4)
Functional & reconstructive (5)
Functional & reconstructive (6)
Functional & reconstructive (7)

The orbits are the anatomical spaces that contain the eye and the tissues surrounding it, such as muscles, fat, arteries, and nerves. Each orbit is located in the skull and is surrounded by bones. These bones make up the four walls of the orbit: the roof, floor, medial wall and lateral wall. The orbital walls closely resemble a slanted, four-sided pyramid that becomes narrow as it approaches the backside of the eye.
The orbital roof separates the eye from the brain. This triangular-shaped wall is thin and may rupture with trauma, allowing the brain to occupy part of the orbit. Tumors of the brain or meninges can also invade the orbit, causing damage to the eye and surrounding structures. Acute or chronic disorders of the frontal sinuses, such as sinusitis or mucocele, may also affect the orbit if left untreated.
The lacrimal gland is an important organ occupying part of the roof of the orbit. Tumors of this gland represent about 10% of all orbital space-occupying lesions. A lacrimal gland tumor may be benign or malignant. Benign lesions are more common and have a good prognosis. On the other hand, cancer of the lacrimal gland is very aggressive and has a poor prognosis. Tumors of the lacrimal gland are covered in another section of this website. https://www.artefacial.com/services/lacrimal-gland-tumors/
The main condition that affects this wall is fracture secondary to trauma to the eye. This happens very commonly after a fist hitting the eye, trauma from a golf ball or an automobile accident. Orbital floor fractures may be managed conservatively in most cases, meaning they do not require an operation. However, some cases in which the eye muscles are trapped in the bone or the fracture is too large may require surgery.
The medial wall of the orbit is so thin that it is compared to a sheet of paper (the medical term is lamina papyracea). This wall separates the eye from the nose and ethmoidal sinuses. Because the nose is not sterile, meaning that it has bacteria, a rupture of this wall can cause an acute infection of the orbit and severe damage to the eye. In fact, the most common cause of infections of the orbit is spreading of an infection in the nasal sinus, located next to the medial wall. These infections are so serious that they may even put the patient’s life in danger if not treated quickly.
The lateral wall of the orbit is the toughest, because it protects the eye from trauma to the side of the face. It requires a big impact to fracture the hard bones in this area. Fractures of the lateral wall may be seen in high-speed automobile accidents.
A tumor can originate from any tissue in the orbit. Fat, blood vessels, or muscle cells may grow abnormally and produce a mass around the eye. The lacrimal gland and the optic nerve can also transform into a tumor. Tumors of the orbit are classified by the tissue where they originate, whether they are benign or malignant, and whether they are caused by inflammation or not. The symptoms of an orbital tumor will depend on the its type, but, as a rule, the patient will experience restriction in eye movement, double vision, discomfort or the eye projecting outward.
Benign tumors of the orbit may be inflammatory in nature or secondary to an abnormal growth of a tissue. Inflammatory masses are more common and should be ruled out first. These tumors tend to cause pain, discomfort and protrusion of the eye.
Inflammation of the orbit is relatively common. It may be secondary to an autoimmune disease, such as Sarcoidosis or Graves’ disease, or an infection in the orbit. Graves’ disease is the most common cause of acute and chronic inflammation of the orbit. This condition affects the muscles around the eye and the fatty tissue. Clinically, it causes the eyes to become red and bulge outward. This condition is described in another segment of this website. https://www.artefacial.com/services/thyroid-eye-disease/
Acute inflammation of the lacrimal gland is another cause of a mass in the orbit. This condition is called dacryoadenitis. Patients experience pain around the eye and inflammation of the outer part of the eyelid. The diagnosis of dacryoadenitis can be made clinically, based on symptoms and signs, or it may require taking a biopsy of the tissue. The treatment of this condition consists of administering oral or intravenous steroids.
Infections of the orbit are very serious conditions that cause acute inflammation of the eye and surrounding tissues. The infection usually originates in the skin of the eyelids or the nasal cavity and spreads to the orbit via blood vessels or the orbital walls. Acute sinusitis can cause a rupture of the medial wall of the orbit and the infection may spread to the area surrounding the eye, causing the it to protrude and become immobile. This infection may produce an abscess which, if not treated, can spread to the brain and put the patient’s life in danger. Patients with an orbital infection must be hospitalized and treated with intravenous antibiotics. If an abscess forms, it must be drained by the orbital surgeon.
Not all benign tumors in the orbit are inflammatory. Some masses grow from tissues in the orbit such as the lacrimal gland, fat or blood vessels. These masses may cause discomfort, protrusion of the eye, and restriction in eye movements. They normally grow slowly and cause minimal pain. Non-inflammatory masses that are benign have a very good prognosis, unless the mass grows excessively and is not removed on time.
Cancer of the orbit is less frequent but has a worse prognosis than non-cancerous tumors. These growths may be primary, meaning that they originate in the orbit, or secondary, meaning that the cancer has spread to the orbit from a distant site. The lacrimal gland is one of the more common sites for primary malignant tumors in the orbit. These tumors usually have a very bad prognosis. On the other hand, lymphoma is a good example of cancer that may cause metastasis to the orbit.
Malignant tumors of the orbit will usually cause more pain and discomfort than benign growths. Patients may notice protrusion of the affected eye, double vision or significant inflammation. If left untreated, the cancer may spread to other organs in the body or cause irreversible damage to the eye.
Orbital lymphoma. This cancer is more common in older patients. The tumor grows from white blood cells in the lymph nodes. It may originate in the orbit (primary) or may spread from a distant site, such as the lungs or the neck. Lymphoma of the conjunctiva has a characteristic reddish-pink color on clinical examination, called a salmon patch. To make the diagnosis, a biopsy of the tumor is taken by the surgeon and analyzed by a pathologist with experience in orbital tumors. Treatment requires chemotherapy or radiation, in most cases, and must be managed with an oncologist.
Cancer of the lacrimal gland. Primary malignant tumors of the lacrimal gland represent about 50% of all lacrimal gland tumors. Adenoid cystic carcinoma is the most common orbital epithelial cancer. These tumors cause restriction of eye movements, pain and bulging of the eyeball. They are very aggressive and require excision and management by an oncologist. Unfortunately, the prognosis is very poor.
Metastasis from distant sites. Cancer in the orbit may grow due to seeding of malignant cells from another organ, such as the breast, lung, and prostate. Malignant melanoma of the eye can also spread to the orbit. Orbital metastasis usually carry a poor prognosis and a short survival rate. Treatment is always managed in conjunction with an oncologist.
Severe trauma to the orbit or an orbital tumor may cause a person to lose vision in one eye. Certain ophthalmologic conditions such as terminal glaucoma, high myopia, and retinal detachment may also cause permanent and irreversible blindness. If the eye has no function but does not cause any pain or discomfort, the person may choose to keep the eye. On the other, a blind, painful eye should be removed to improve the patient’s quality of life. In this case, an orbit specialist will perform a surgery to remove the eye and reconstruct the socket.
There are two options to surgically remove an eye:
An evisceration is a procedure where the contents of the eye are removed, but the scleral shell and the muscles of the eye are left intact. This is probably the most common operation to remove an eye. It is usually performed to reduce pain or to improve cosmesis in a blind eye. After removing the contents the eye, an orbital implant is placed in the scleral shell to restore volume. Six to eight weeks later, an ocular prosthesis is designed by an ocularist and placed into the socket to simulate the normal eye.
An enucleation is an operation that involves removal of the whole eye, including the scleral shell (the with covering of the eye); only the muscles of the eye are left in the orbit. This procedure is indicated for ocular tumors such as malignant melanoma. It may also be done in acute trauma, when an eye has incurred severe damage. In an enucleation, the orbital implant is sutured to the eye muscles and not to the sclera. An ocular prosthesis is placed in the socket two months after the operation.
After removing an eye, a patient will wear a prosthesis that imitates the color, dimensions and shape of the healthy eye. The prosthesis should feel comfortable and fit properly in the socket. There should be little, if any, secretion. A prosthesis should be removed and cleaned about once a week and should be polished every 6 months or so.
Some patients may experience problems wearing the prosthesis. This may be due to improper fitting, extrusion of the orbital implant, or inflammation of the socket. Inflammation of the eye socket will cause chronic secretion and discomfort and may also lead to scarring, which will shrink the socket and will make it impossible to hold a prosthesis. In these cases, the orbital surgeon will have to reconstruct the socket to restore volume and prevent more scarring. Expansion of the socket with implants or grafts will allow the socket to accommodate a new prosthesis.
Some patients have loss of volume in the socket after the removal of an eye, even while wearing a prosthesis; this is called sunken sulcus syndrome. These patients have deep-set eyes that look cadaveric. The upper eyelids are very droopy in most cases. There are several options to treat this condition. One alternative it to restore volume by injecting hyaluronic acid fillers or fat to the orbit. Another option is to surgically reconstruct the socket and add volume with a bigger implant of a dermis fat graft. Once the volume is restored, a prosthesis can be placed into the socket.
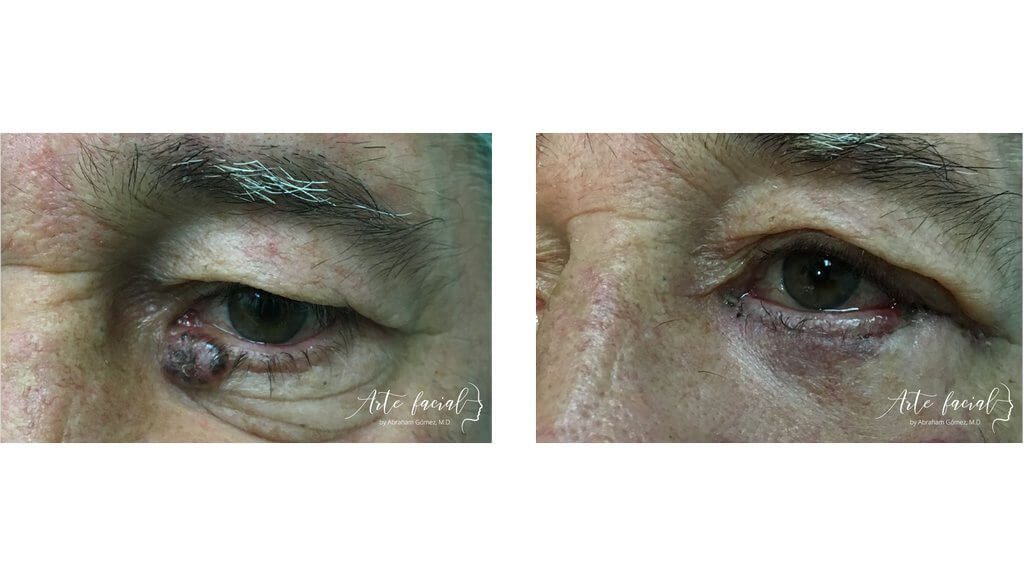
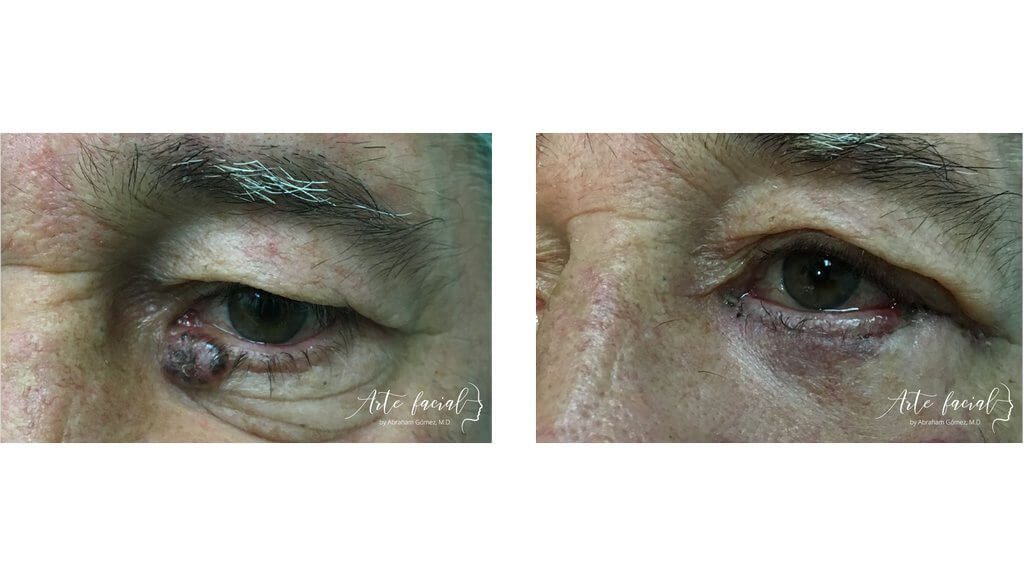
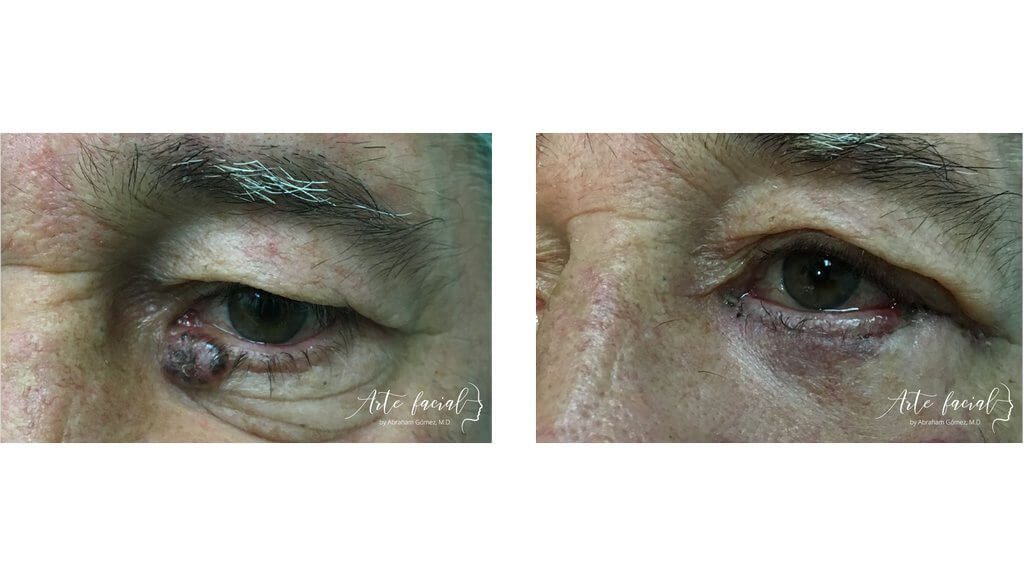
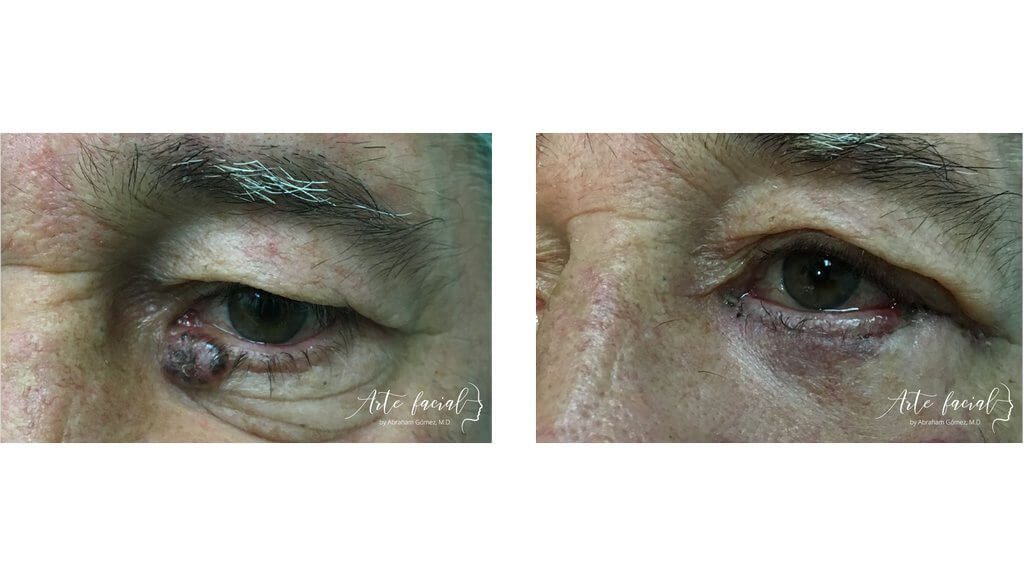
Before
After


+506 7032-5570
Abraham Gómez, MD
Hospital Clínica Bíblica, Omega Building, 2nd floor
Loras Medical, Torre Las Loras, main floor
ARTE FACIAL
ARTE FACIAL
Visit us at our new office! 25% off on your consultation at Loras Medical. Book here (Valid Until December 15, 2023.)
Please fill out the form below to schedule a virtual consultation with Dr. Gomez.