A teary eye is a very common condition seen in an oculoplastic surgeon’s medical practice. Teary eye has several causes, one being a lacrimal duct obstruction. Now, to understand the mechanism of a tear duct obstruction, it is important first to know a little bit about tear duct anatomy.
Tears are produced by several glands, of which the lacrimal gland is the most important. Without a healthy tear film, our cornea would dry out, become scarred or infected.
After the tears have done their job in lubricating the eye, they exit through a drainage system. This tear duct system starts in the eyelids, in very small canals called canaliculi. The tears travel from the canaliculi to a tear reservoir called the lacrimal sac. From here, they go down to the nose. The nasolacrimal duct connects the upper tear duct (located in the eyelids) to the nose. It is here that most tear duct obstructions ensue.
Tear duct obstruction: who does it affect and why does it happen?
Acquired tear duct obstructions are very common. They are much more frequent in older females. Although the exact cause of the obstruction is not known, it is thought that it is related to scarring of the lower portion of the duct. A hormonal component has also been surmised, which explains why this is more common in the aforementioned age group.
What are the main symptoms of a tear duct obstruction?
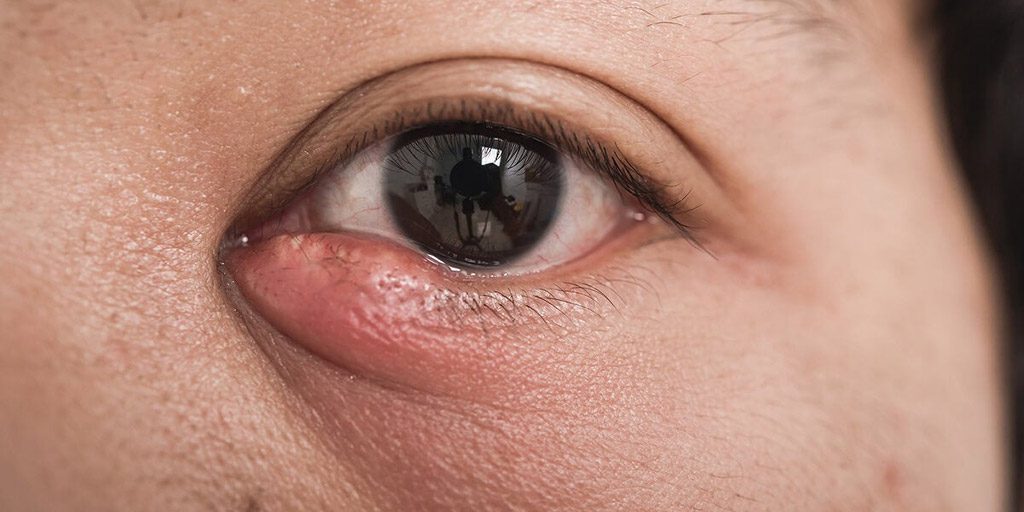
Tearing, medically known as epiphora, is the main and most common symptom of a tear duct obstruction. However, some patients will also complain of a mucous or purulent discharge in the affected eye, especially in the mornings upon waking. This discharge signals a chronic infection of the tear sac secondary to the obstruction. Unfortunately, the infection may become acute, causing an abscess of the tear sac (acute dacryocystitis). This infection must be treated promptly since it may spread to the orbit and may compromise the patient’s vision and health otherwise.
In summary, a tear duct obstruction may simply be a bothersome condition that causes tearing, or it may become rapidly severe, jeopardizing a patient’s health in some cases. The best course of action is to consult your lacrimal surgeon to make the right diagnosis and offer the best treatment.










 |
|